Site-Specific Antibody Prodrugs via S-Arylation: a Bioconjugation Approach Toward Masked Tyrosine Analogues
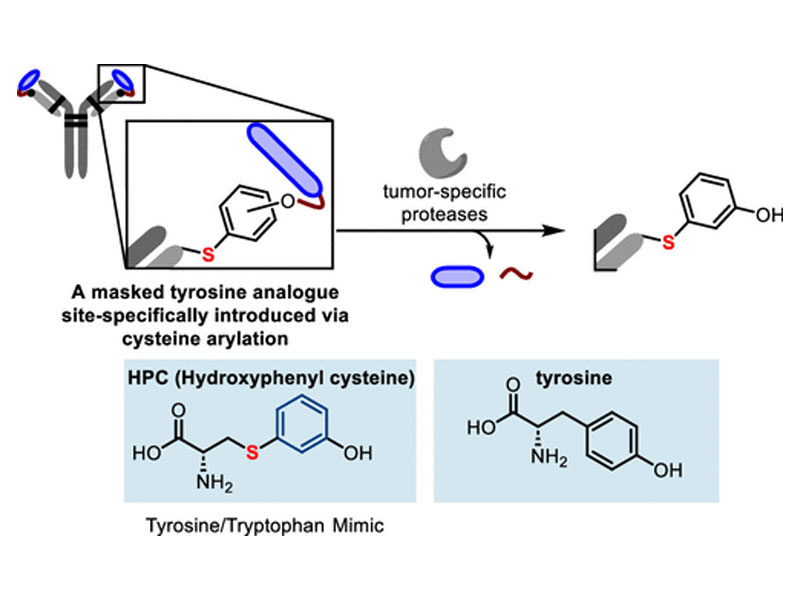
Site-Specific Antibody Prodrugs via S-Arylation: a Bioconjugation Approach Toward Masked Tyrosine Analogues
Jason TaoHeemal H. DhanjeeMichael W. Gribble JrVeronika KottischJacob RodriguezJoseph S. BrownHolly SchmidtJuhi JunejaFabienne DenhezPeter S. LeeDaša LipovšekStanley KrystekYihong ZhangPatrick BousquetYong Zhang*Bradley L. Pentelute*Stephen L. Buchwald*
Abstract
The utility of antibody therapeutics is hampered by potential cross-reactivity with healthy tissue. Over the past decade, significant advances have been made in the design of activatable antibodies, which increase, or create altogether, the therapeutic window of a parent antibody. Of these, antibody prodrugs (pro-antibodies) are masked antibodies that have advanced the most for therapeutic use. They are designed to reveal the active, parent antibody only when encountering proteases upregulated in the microenvironment of the targeted disease tissue, thereby minimizing off-target activity. However, current pro-antibody designs are relegated to fusion proteins that append masking groups restricted to the use of only canonical amino acids, offering excellent control of the site of introduction, but with no authority over where the masking group is installed other than the N-terminus of the antibody. Here, we present a palladium-based bioconjugation approach for the site-specific introduction of a masked tyrosine mimic in the complementary determining region of the FDA approved antibody therapeutic ipilimumab used as a model system. The approach enables the introduction of a protease cleavable group tethered to noncanonical polymers (polyethylene glycol (PEG)) resulting in 47-fold weaker binding to cells expressing CTLA-4, the target antigen of ipilimumab. Upon exposure to tumor-associated proteases, the masking group is cleaved, unveiling a tyrosine-mimic (dubbed hydroxyphenyl cysteine (HPC)) that restores (>90% restoration) binding affinity to its target antigen.